
Treatment standards in Israel’s hospitals will fall and the chances of dying of COVID-19 will increase in just over three weeks unless the infection rate is slowed, a Hebrew University research team has concluded.
Besides the pessimistic predictions on patient care, the analysts said 100 more coronavirus deaths are likely before the end of July.
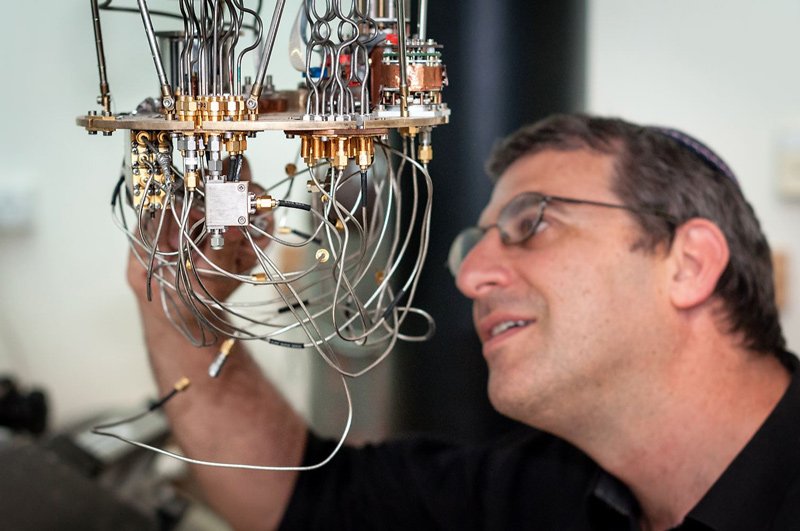
Nadav Katz of the Hebrew University of Jerusalem’s Racah Institute of Physics said that if infections spread at current rates, within 24 days there will be more than 1,000 patients in moderate and serious condition, which is “roughly the capacity of our healthcare system.”
He told The Times of Israel that his team used statistical models and found that past the stage of 1,000 serious and moderate patients, a figure believed to be around the corner, hospitals will still find beds, but “the strain becomes unbearable” and “the level of treatment and morbidity would get much worse.”
He added: “When a medical system exceeds its capacity the standard of care goes down and the result is less survival of the critically ill.”

“It’s not because of equipment and infrastructure but because of trained staff,” he added. “It’s not a matter of buying more ventilators, but rather having a team that can use them.”
Katz is part of a specialist Hebrew University stats team, together with Hadassah Medical Center doctor Ronit Calderon-Margalit; epidemiologist Ran Nir-Paz, an infectious diseases expert; and several other scholars.
The team has representation on a Health Ministry advisory committee.
Katz said that the combined number of moderate and serious patients is doubling every 12 days. It currently stands at 274. If it doubles within 12 days, raising the prospect of another doubling 24 days from now to more than 1,000, it will ring alarm bells, he said.
“When we’re at half the capacity, that’s already starting to be too late,” said Katz. “It won’t then be a point where you can push a button and turn things around.”
Katz’s assessment of health service capacity, and his fear of a drop in care levels, is shared by some professionals in hospitals.

“Before coronavirus we had 758 intensive care beds in Israel and we’ve built a few more so the capacity is probably 1,000 at this point,” said Zeev Feldman, deputy president of the Israeli Medical Association and pediatric neurosurgery at Sheba Medical Center in Ramat Gan.
Feldman said he is inclined against “doomsday prophecies,” and thinks there is a good chance that restrictions enacted at the start of the month will pay off and prove to have slowed cases. Nevertheless he is carefully monitoring the number of serious cases, which in his view provides a better indicator of the situation than Katz’s combined serious-moderate count.
Serious cases currently stand at 172, reflecting a doubling in the last 10 days. Feldman said that if this number rises to 300, patients “may get care that is less good,” and if it hits 500 serious cases, which he regards as national capacity, people will “of course” get a lower level of care.
“They will be treated by less trained personnel,” he commented.

“The intensity of care a coronavirus patient needs is far beyond that of a regular intubated and ventilated patient,” Katz said, and the pool of staff with the appropriate training is small.
Katz’s team says that the moment of truth will come this weekend, when it will be possible to assess whether new restrictions enacted at the beginning of the month had a positive impact. The rationale is that patients tend to end up in hospitals around two weeks after infection, so if the July 2 restrictions reduced infection rates, that should be felt on wards in the coming days.
He said that if an improvement isn’t seen, the government should enact more restrictions, and the public should step up efforts to slow infection. “It’s not a Greek tragedy, the future isn’t written yet,” he said. “We have the power to turn it around and dodge this bullet.”
Katz’s conclusions stand in stark contrast to the optimistic assessment given by a prominent Jerusalem doctor on Thursday.
“I don’t think we’ll be overwhelmed. We are far from our reserve,” Prof. Jonathan Halevy, president of Jerusalem’s Shaare Zedek Medical Center and a member of a Health Ministry public information team, said regarding the capacity of the country’s hospitals. “I’m confident about the next few months. I’m also optimistic about the winter.”