Animal testing is cruel and often unnecessary. But the FDA forces drugmakers to do it.

Times, and technologies, are changing. With growing momentum in the movement to stop harmful animal testing and major advancements in alternative research methods, it’s time to right the wrongs of the past.
Animal testing is not nearly as accurate as scientific alternatives, and certainly much less humane. Yet, the Food and Drug Administration requires it for certain approvals. We’re here to change that.
Researchers from the Hebrew University of Jerusalem recently submitted for FDA approval the first drug developed using high-tech research tools and absolutely no animal testing. This is a major breakthrough and should become the rule at the FDA, not the exception.
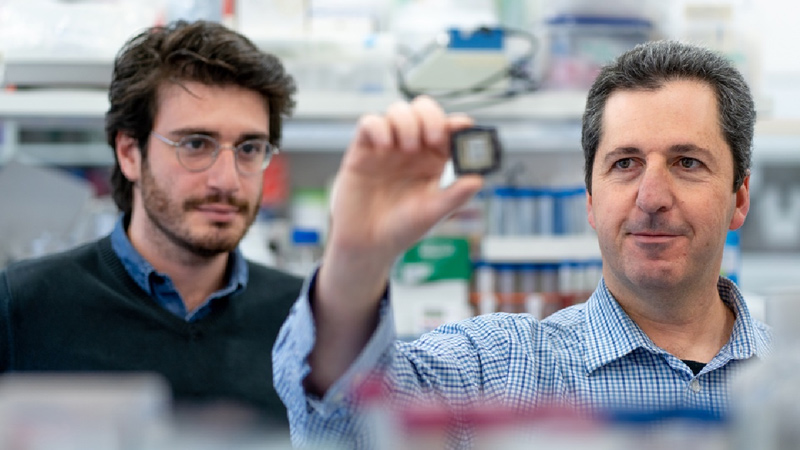
“To our knowledge this is the first time a drug is taking this step without animal testing, and the reason is that we have eliminated this need by using our ‘human on a chip’ technology,” said Professor Yaakov Nahmias, lead author.
“This is the first demonstration that we can use such technology to circumvent animal experiments, and this could lead to faster, safer and more effective drug development.”
“We’ve done it without a single animal.”
To mimic how the drugs would interact in humans, they used human kidney spheroids – a spherical cell culture – embedding microsensors to analyze the metabolism of the tissue. This biological “chip” allowed them to test their therapy and get real-time results without the use of animal models.
With this being the first drug to go through to approval without animal testing, if successful, this study could be a breakthrough in reducing the number of animals used in labs. With various technologies that simulate drug interactions leaping to the foreground recently – including organoids, computer simulations, and more – it may be very possible that the future of animal-free drug testing is closer than we think.
As many as one-third of all dogs subjected to experiments each year are tested on to fulfill outdated regulatory requirements from the FDA and other federal agencies. As White Coat Waste Project has documented, in some of the standard tests the FDA compels companies to conduct, puppies as young as 1 week old are forced to ingest massive doses of experimental drugs, often resulting in convulsion and death.
Animal testing isn’t just inhumane, it’s also incredibly expensive. Researchers at Hebrew University found that while it normally takes four to six years and millions of dollars to bring a drug to clinical trial using animal testing practices, it only took them eight months, at a fraction of the cost, when using science-based testing methods. Estimates say drug development costs could be cut by over a quarter with more expanded use of non-animal testing tools.
Recently, drugmakers have begun developing and embracing new technologies built from human cells and tissues. Researchers from the University of Pennsylvania and elsewhere have shown that these 21st-century methods are more accurate at predicting how drugs will behave in humans than animal tests.
In some cases, the FDA has reportedly allowed companies to bypass some animal testing prior to initiating human trials, leading to the expedited review and approval of several effective COVID-19 vaccines now in widespread use. Yet, in other instances, drugmakers state that they were directed by the agency to conduct unnecessary and expensive testing on dogs without any scientific basis.
Part of the current problem is that FDA rules about what animal tests are actually required are unclear and lack a well-defined and transparent process for companies to propose alternatives. The agency has repeatedly failed to answer Congress’ questions about this.
So, drugmakers often end up conducting needless animal tests, even when they would prefer to use more effective and efficient alternatives. The National Institutes of Health estimates that over 90 percent of drugs fail in human trials because animal tests don’t accurately predict their safety or effectiveness.
The NIH admitted that “animal models often fail to provide good ways to mimic disease or predict how drugs will work in humans, resulting in much wasted time and money while patients wait for therapies.” This problem is particularly apparent now as we continue confronting the COVID-19 pandemic. One team of researchers recently remarked, “Scientists worldwide struggle to identify suitable animal models to study SARS-CoV-2. … Especially for human diseases with an urgent medical need and a lack of suitable in vivo models, human-based models may expedite clinical translation.”
Americans want the government to do better. A March national poll of 1,000 voters conducted by Lincoln Park Strategies found that 64 percent of people believe drug companies should be allowed to use alternatives to animal testing whenever possible. So do we.
That’s why we’re working together to pass the bipartisan Alternatives to Animals for Regulatory Fairness Act — the AARF Act, for short — to update federal law to clearly allow drugmakers to use alternatives to animal testing to meet FDA drug screening requirements.
For the benefit of human patients and lab animals, companies should be allowed to innovate and use the most cutting-edge drug development tools instead of being compelled by the government to abuse animals in painful, outdated and inefficient experiments.
- Rep. Brendan F. Boyle is a Democrat representing Pennsylvania’s 2nd District. He serves on the House Budget and Ways and Means committees.
- Justin Goodman is the vice president of advocacy and public policy at the White Coat Waste Project, a 3-million-member taxpayer watchdog group.
Article originally appeared on Roll Call.