Isaiah (Shy) Arkin is a professor of Structural Biochemistry at the Hebrew University of Jerusalem, whose research, among other achievements, has shed new light on the inner workings of viruses. The Times of Israel spoke to him to try to understand more about the coronavirus, how it compares to other viruses, how its spread might stop or be stopped, and how worried humankind should be about it.
He stressed that he didn’t have all the answers to our questions.
The Times of Israel: First, please explain to me what your expertise is as it relates to the current coronavirus crisis.
Prof Shy Arkin: Okay, so let me first say that I am not a physician, nor am I an epidemiologist, and I may not even be considered a virologist per se. What am I then? I am a biochemist and what I study are the mechanisms in which viruses regulate their salinity and acidity. So I am a molecular expert on several different parts of viruses.
The two staple viruses that we have studied for close to two decades are influenza and SARS. We have characterized several important components in these viruses.
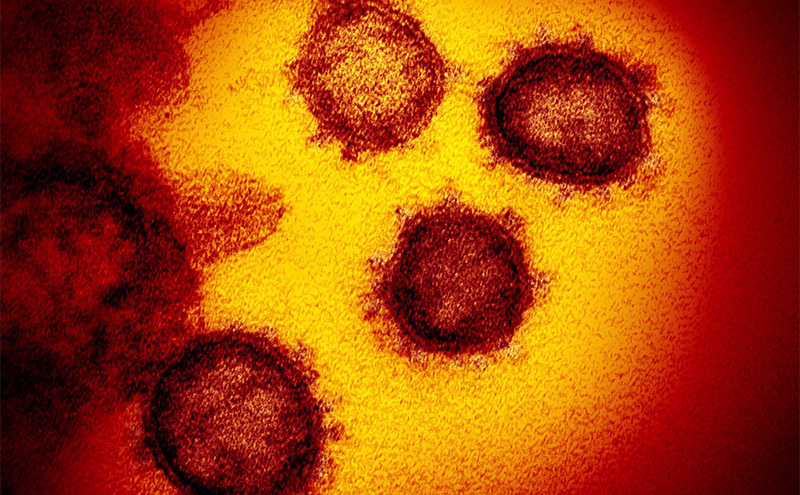
And to our amazement, this new virus, which is now called SARS Coronavirus 2, is incredibly similar to SARS Coronavirus 1, that was responsible for the SARS epidemic in 2002-2003 .
Now we can harness all of the expertise and knowledge that we had, to try to find inhibitors to this virus, which is precisely what we’re doing.
Q: So we’re trying to find inhibitors. How does that relate to what we’re also told, which is that a vaccine is probably a year away?

Okay. So let’s take a step back and ask ourselves the following question: How does one deal with viruses?
There are two common routes and one slightly less common, other than simple supportive care.
The most common route is vaccination. It takes a while to develop a vaccine.
I think it’s fair to say that the efforts that are currently underway around the world are the fastest ever. But it’s still very, very unrealistic to state that we will have a vaccine within the next few months. It simply takes longer than that, for a variety of reasons.
Another route that people are taking, and that’s the route that I’m taking, is to look at drugs that inhibit viruses. So, for example, there are very effective drugs against HIV, the causative agent of AIDS. There are no vaccines against AIDS. They are somewhat effective drugs against hepatitis C. There are no vaccines against hepatitis C.
Some viruses have both. Influenza has drugs — you might have heard about Tamiflu — and of course, everyone knows about the flu shots. So there are viruses that you can use this method or that method.
The last method, which we are not doing, which is not as common, is an antiserum. That’s the sort of thing that when you get bitten by a snake, you rush to the clinic and then what they essentially give you is antibodies that someone else generated for you. Often it’s a large animal like a horse or that sort of thing. In the first SARS epidemic in 2003, people tried that to an extent. They literally took antibodies or serum from the blood of someone who recovered from that disease, and gave it to someone who was currently sick. They did that a few dozen times, if I’m not mistaken. But that’s not a very common route.
Q: Of the two main routes — the one that you are researching (drugs), and the vaccine, which do you think is going to get there first?
Very difficult to say. That all depends on the following. If what we do is we identify in our laboratory a brand new chemical, a chemical that has not been approved for use in humans — you’re talking about a long period of time, you’re talking about several years. And the reason for that is that you need to look at the toxicology of that. And that’s not a very simple thing to do.
However, what is far more common today is the process of what’s called repurposing. Repurposing means let’s take a drug that has been approved for one disease, and then suddenly use it against this disease. There’s hundreds, if not thousands, of drugs that have been approved for use in humans against a variety of different diseases.
If something has been approved, it means that its toxicology has been characterized. And it doesn’t really matter if the drug that you’re taking is against liver disease, baldness or high blood pressure. The toxicology is toxicology is toxicology. So if you suddenly find, wow, this chemical is also efficacious against COVID-19, ah, we could use this — and therefore we can bypass a tremendous amount of work that is required in clinical trials. You do need a bit of regulation, but it’s far more rapid.
Q: If a vaccine is a year away, and the drug approach could be faster or slower, the worst-case scenario that the watching world is looking at is a year until there’s some kind of treatment. Correct?
No! The worst-case scenario is we never find anything.
Q: It’s plausible that they won’t find a vaccine fairly rapidly?
We all know of the tremendous mortality and morbidity that AIDS has been exacting from humankind. We have no vaccine.
Hepatitis C is a tremendous problem. We have no vaccine.
If you’re looking for your best-case scenario, it is something beyond a few months. I’m specifically being vague. I don’t want to say six months because people tend to give a lot of importance: ‘Oh, a professor said this. It must be true.’ And we all know that that’s not necessarily the case.
I would say it’s exceedingly optimistic to say a few months. A year is not unrealistic.
However, the upper limit can be never. Because there are viruses… We don’t have a vaccine for SARS. From 2000 to 2003. Now, I don’t necessarily know if it’s because people have lost interest, because there has been no reported case of someone that got SARS since 2003 till today. So interest hasn’t been there.
Q: But that’s because we did find drugs to treat it.
No. There is absolutely nothing to treat any coronavirus. There are vaccines against coronaviruses that affect animals but not against coronaviruses that affect humans.
Q: So SARS just faded away?
Correct.
Q: SARS 1?
Let’s just use a tiny, tiny, tiny bit of the nomenclature: AIDS is the disease; HIV is the virus that causes the disease. SARS is the disease; SARS Coronavirus-1 is the virus that causes the disease. The current disease is called COVID-19 and the virus is called SARS Coronavirus-2.
Q: And we never found a fix for SARS Coronavirus-1?
Or any other human coronavirus for that matter. We know about coronaviruses for a long period of time. They normally cause mild colds in humans. It’s not the major element that causes the common cold; the major element is another virus, called rhinovirus, rhino from nose. But coronaviruses clearly cause mild respiratory tract infections.
In livestock and in birds, they do exact a significant morbidity. So if you’re a farmer, these things do bother you significantly. But to humans, they haven’t been an issue. Again, there are vaccines to some coronaviruses that infect animals.
Q: There is a concern that this virus is of a different order. And you’re saying there are no guarantees that either a vaccine or drugs will be found?
Correct.
Q: That sounds apocalyptic.
No, no, no. I don’t want to elicit any sort of panic. So, first of all, the new virus is very, very, very, very similar to the one that the research community found in 2002-2003. The thing that caused SARS in 2002-2003 is very, very similar — as I said, 80 percent identical — to the thing that’s causing COVID-19. So it’s not as if this is coming out of nowhere.
Having said that, right now, since we have no drugs or vaccinations and nothing is on the immediate horizon, if you wanted to be certain, if you were an insurance agent, you would clearly be able to say we have no insurance with any certainty that we will generate a vaccine or a drug.
This is not going to kill humanity. This is a disease that mostly afflicts the elderly, not that one does not care about the elderly. But to people that are not classified as elderly, this generates a respiratory tract infection that is not very severe, and most people have very mild symptoms.
So the fact that you have a 2 percent or 3 percent mortality rate — that number is driven upwards by the fact that the elderly are far more susceptible to it.
You’re not going to see millions upon millions of people dying. That’s not going to take place.
I mean, look at China. China today has barely any new cases.
Q: So why then, professor, am I living in a country that has just told everyone to stay home. And watching the United States now telling people not to gather in groups of more than 10, having previously sort of brushed this off? And Britain, which was really saying, Nothing to worry about here, all of a sudden telling people…
Fear of the unknown. Fear of the unknown. Very simple.
Let’s imagine three scenarios. Scenario number one, the best case-scenario, is that this disease disappears by the time we finish talking. That’s probably not going to happen.
Another scenario would be what happened with its cousin SARS from 2002 to 2003. That virus, which was more deadly — which could have actually limited its spread, because if something is very virulent, then immediately people rush to the hospital and get quarantined — pretty much disappeared in June , when the conditions were sufficiently hot and people stopped crowding, etc.
And the last scenario is doomsday. Where will we fall? I don’t know.
Q: But you don’t think millions of people are going to die around the world?
I can’t imagine why. China is a quarter of the world’s population, right, give or take, maybe slightly less. Roughly 3,000 deaths in 1.5 billion people… China seems to have plateaued.
Q: 3,000 deaths among 1.5 billion people. And you’re saying that should be some kind of point of reference when we try to work out how worried we should be?
The biggest problem that we don’t know what we classify as asymptomatic people. An asymptomatic person is someone who’s carrying the virus, who might actually be infectious, but doesn’t realize that he or she is carrying the virus. And that’s an issue.
The reason that they were able to to prevent that sort of infection in China is curfew. Curfews are effective. In China, there have been very, very few new cases in the last few weeks. Is that something that we want the world to do? I’ve no idea.
Q: Put what you just said up against that death rate — that 3 to 4 percent death toll among people who are infected?
Again, we don’t know the number of asymptomatic people. That’s the biggest question. The bigger that number is, the better. For example, if you assume that three quarters of humanity actually have the virus within them but are not exhibiting any pathology whatsoever, that would be excellent. That’s a good thing.
Q: That means the death rate among those who are infected is, in fact, massively lower, if there are lots and lots of people who are asymptomatic?
Correct.
The death rate, the mortality rate, is close to 4 percent.
Q: But that’s a rate calculated among those who know they are infected?
A rate those cases that have been confirmed of COVID-19, yes.
Q: Whereas it is reasonable to believe that an accurate rate among those who are infected would actually be much lower?
Could very well be, yes.
One of the limiting factors, as you know, has been the availability of tests. If your name is not Bibi or Donald, the probability of them testing or relegating some of these precious tests to people that are not clearly sick, is vanishingly small.
If we had a test that could be administered to every every individual, then we would have an immediate answer. We don’t. And that’s the problem.
Q: Is this a virus that is able to adapt, to change, in order to beat efforts to stop it? Or do we not know that?
First of all, if we want to be a bit optimistic, lots of people have recovered from this virus in China. Lots. And by the way, recovery does not mean that you don’t die. Recovery means you’re no longer infectious, and you are not exhibiting any symptoms. So that’s really good. Recovery means this is someone that you can go ahead and hug in public.
There have been 56,000 people in China, out of 80,000, that have recovered completely. So this is not as bad of a killer. But there is a trajectory. Where will this end? We don’t know.
Q: How should we compare it, in terms of the danger it poses, to flu, for example, or to smoking , for example?
Well, flu every year just in the United States kills about 60,000 people. So in terms of the death toll, flu is much, much, much worse. Even in China, flu this season — I’m not talking about last year — this year has killed far more people than COVID-19.
But the thing about flu is that it’s a danger that you’re familiar with. You know the rough extent of it. And in that respect, it’s not something that’s unexpected. When you see something that’s rising, you always wonder, you know, when is this going to stop and where is this going to stop? In flu, you know. Obviously, smoking kills lots of people as well. But the thing is, you can’t just say, Oh, that’s much worse, because this thing is additive to that. It’s not replacing those fears.
Q: I just want to come away from this conversation able to convey a sense of how concerned people should be, and how smart or otherwise the world’s political leadership is proving in handling this.
Well, I think you’re pushing me beyond my expertise. I’m not an epidemiologist, but as a scientist, I am able to read and understand numbers perhaps in the way that the layperson may not be able to. But the impact on the psychology and on politics is not something that I feel very comfortable commenting on.
Q: I understand and I absolutely respect that. Tell me, what are you telling your family to do? What are you doing in terms of precautions?
Following the guidelines, so I’m not going to any crowded places. I’m driving the car. If I want to have a bit of fresh air, then I’ll go to a short hike in the forest. It’s simply following the guidelines. We have not gone to the supermarket to start hoarding food.
It’s similar to asking the insurance agent, you know, Do you buy earthquake insurance even though there hasn’t been an appreciable earthquake in Israel in a significant amount of time? People take different attitudes.
We all know that we’re going to die. Does everyone take exactly the same life insurance? No, they don’t.
There is no reason whatsoever to assume that my opinion is better than anyone else’s, other than the fact that I understand some of the molecular details about this virus far better than most people in the world. I don’t think that qualifies me to make any other judgments.
Q: I understand. You, like everybody else, are following the guidelines. But as a scientist, can you sum up for people, as they dutifully do what they are told to do, how worried or not worried they should be? From the scientific perspective.
It’s too subjective. It’s very difficult to say. This is clearly not doomsday. Humanity will not vanish due to this virus. There is no reason to assume that that will take place.
But as they say, you know, every death, every loss of life, is a world in itself.
We still drive to work. And that’s probably the most dangerous activity that any Israeli does. Yet we continue doing it… What is extreme to one person may not be extreme to another. I don’t know.
Q: Is there anything I should have asked you that I haven’t asked you?
Well, to put things from another perspective:
I’m dodging your questions because I don’t have an answer. One thing that I always recall is an amusing anecdote that’s used by Nobel Prize winner Daniel Kahneman from the Hebrew University, on the psychology of decision making: Someone goes to a doctor with a particular problem. The doctor tells him, oh, fantastic, I have a procedure that will cure this by 90 percent. The patient says: Excellent procedure — sure. Sign me up.
That individual might choose to go to a different doctor. And that different doctor might say, oh, I have a procedure, but there’s a 10 percent failure. The patient says, That’s a terrible procedure. Why would I use that?
Obviously, we realized both doctors are saying exactly the same thing. And yet the patient is acting completely differently.
Facts are one thing. And the way that people react to them and make evaluations is entirely different. That’s why I don’t necessarily think that scientists who are able to provide rigorous numbers, and epidemiologists, etc., might necessarily be effective in either calming people down or hastening their panic.